Narcolepsy is a rare and chronic neurological disorder characterized by instability in sleep-wake regulation. marked by chronic excessive daytime drowsiness (EDS) and disrupted nighttime sleep. Individuals with narcolepsy experience sudden sleep attacks that may last from a few seconds to several minutes and can occur multiple times a day. The condition is thought to be autoimmune, involving the destruction of brain cells that produce hypocretin, a peptide critical for regulating sleep and wakefulness. Narcolepsy disrupts the normal sleep cycle, causing REM sleep to begin abnormally early. There are two types of narcolepsy as classified by the International Classification of Sleep Disorders, Third Edition (ICSD-3):
- Narcolepsy Type 1 (NT1): Cataplexy, low levels of hypocretin.
- Narcolepsy Type 2 (NT2): Similar to NT1 but without cataplexy or low hypocretin levels.
The disorder affects approximately 1 in 2,000 people, though many cases remain undiagnosed or misdiagnosed.
Clinical Description and symptoms
| Classification Level | Disorder |
| Prevalence | 1/2000 -1 /5000 |
| Age of Onset | Adolescent, Adult, Childhood |
| Inheritance | Unknown |
Symptoms typically start between ages 10 and 30 and are lifelong. Diagnosis often takes about 10 years from symptom onset. Non-specific signs may include hypnagogic hallucinations, sleep paralysis, disturbed nocturnal sleep, and weight gain in children. The disorder is linked to the loss of orexin/hypocretin neurons in the lateral hypothalamus, resulting in low hypocretin-1 levels in cerebrospinal fluid. An autoimmune origin is suspected, with genetic factors (e.g., the HLA-DQB1*0602 allele) playing a role, though this remains unproven Excessive Daytime Sleepiness (EDS): Overwhelming urge to sleep, particularly in monotonous situations, leading to sudden sleep attacks and lapses in attention. Symptoms include:
- Automatic Behaviors: Unconscious actions performed while drowsy, such as writing meaningless text.
- Disrupted Nighttime Sleep: Frequent awakenings, excessive physical movements, and sleep apnea.
- Sleep Paralysis: Inability to move while falling asleep or waking up.
- Sleep-Related Hallucinations: Vivid visual or sensory experiences occurring while falling asleep (hypnagogic) or waking up (hypnopompic), sometimes with sleep paralysis.
- For Narcolepsy Type 1 (NT1), an additional symptom is:
- Cataplexy: Sudden loss of muscle control triggered by strong emotions, lasting from seconds to minutes, affecting both sides of the body.
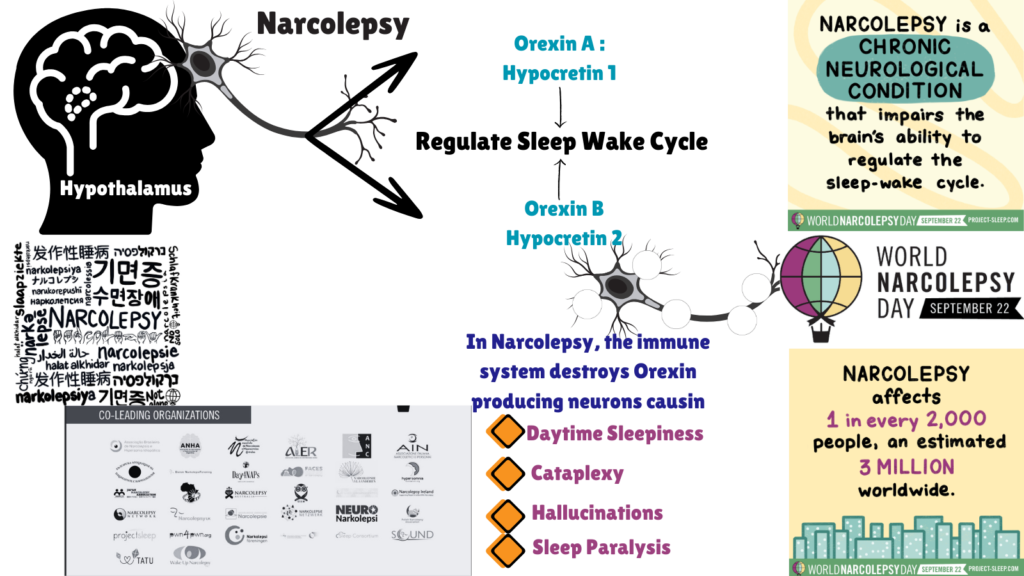
Image: Causes, Prevalence and Symptoms of Narcolepsy
Diagnosis and Treatment
To diagnose narcolepsy, clinicians rely on a combination of clinical symptoms, specific findings from polysomnography, and cerebrospinal fluid analysis for hypocretin-1 levels. A diagnostic polysomnography usually reveals at least two sleep onset rapid eye movement episodes SOREMPs) and an average sleep latency of less than eight minutes. Low cerebrospinal fluid hypocretin-1 levels (<110 pg/ml) can confirm the diagnosis. Differential diagnosis involves ensuring that cataplexy is characteristic; without it, other causes of excessive daytime sleepiness, such as chronic sleep deprivation or idiopathic hypersomnia, should be considered. Genetic counseling is rarely needed, as familial cases are uncommon, and inheritance patterns are unclear. Management focuses on symptomatic treatment since the loss of orexin neurons is irreversible. First-line medications include modafinil, pitolisant, and sodium oxybate, with second-line options like methylphenidate and amphetamines. Sodium oxybate is particularly effective for both daytime sleepiness and nighttime disruptions. Good sleep hygiene practices, including regular naps and consistent sleep routines, are also recommended. Although narcolepsy can significantly impact academic and professional performance, the condition often remains stable, with potential improvements in symptoms over time, though nighttime sleep quality may deteriorate with age.
For more on therapeutics against this disease, stay tuned for N for Narcolepsy Part II. Meanwhile, click here for more available resources and support groups for Narcolepsy.
Dr. Malini Gupta, Ph.D.
Sources
- https://www.orpha.net/en/disease/detail/2073
- https://www.sleepfoundation.org/narcolepsy
- https://rarediseases.org/rare-diseases/narcolepsy/
- Figure has elements from – https://project-sleep.com/
Disclaimer
The editors take care to share authentic information. In case of any discrepancies please write to newsletter@medness.org
The sponsors do not have any influence on the nature or kind of the news/analysis reported in MedNess. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of MedNess. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products as they are based only on very limited and dated open-source information. Assumptions made within the analysis are not reflective of the position of anyone volunteering or working for MedNess. This blog is strictly for news and information. It does not provide medical advice, diagnosis or treatment nor investment suggestions. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
MedNess is a part of STEMPeers® which is a 501(c)(3) organization registered in PA as PhD Career Support Group. The organization helps create a growing network of STEM scientists that is involved in peer-to-peer mentoring and support.



