Multiple Myeloma is a rare cancer that arises from plasma cells, a type of white blood cell produced in the bone marrow. These cells become malignant, proliferating uncontrollably and leading to tumor formation primarily in the bone marrow. When only a single tumor is present, the condition is called solitary plasmacytoma. When multiple tumors are present or plasma cells comprise more than 10% of the bone marrow, it is classified as multiple myeloma.
The exact cause of multiple myeloma remains unknown, with no specific avoidable risk factors identified. However, several risk factors increase the likelihood of developing the disease:
- Age: Risk rises significantly after age 65.
- Gender: Men are slightly more likely to develop multiple myeloma than women.
- Radiation Exposure: Prior radiation exposure may elevate risk.
- Family History: Having a first-degree relative with multiple myeloma increases risk, though this is rare.
- Occupation: Working in certain industries, such as oil-related fields, may be linked to a higher risk, although evidence is not conclusive.
- Obesity: Being overweight might be a risk factor.
- Pre-existing Plasma Cell Disorders: Conditions like monoclonal gammopathy of undetermined significance (MGUS), solitary plasmacytoma, or smoldering myeloma increase the risk.
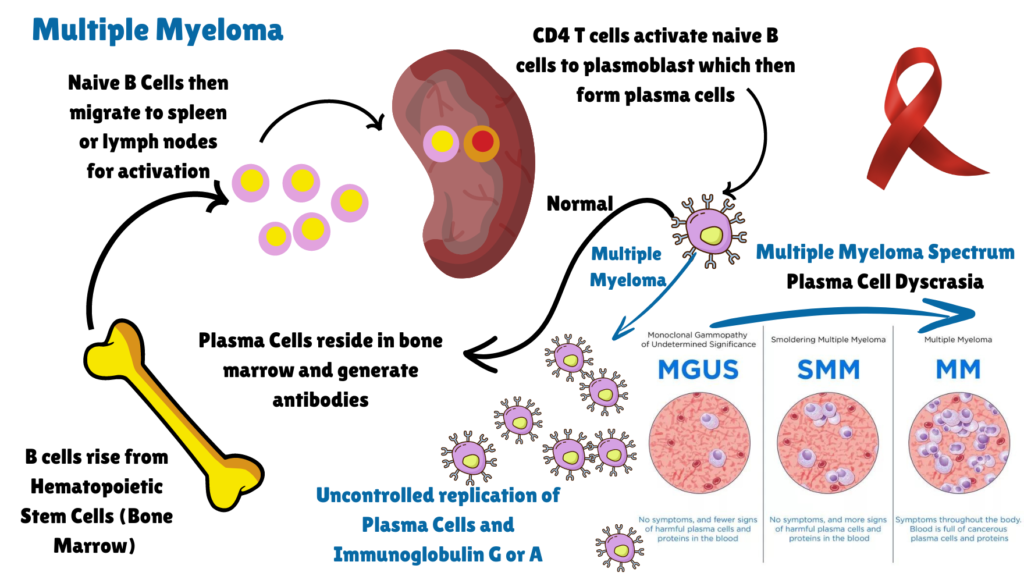
Image: Disease Progression and Symptoms of Multiple Myeloma
Clinical Description and symptoms
| Classification Level | Disorder |
| Prevalence | 1-5/10,000 |
| Age of Onset | Adult Onset |
| Inheritance | NA |
Plasma cells are integral to the immune system as they produce immunoglobulin proteins (M-proteins), which are antibodies that help fight infections. In multiple myeloma, an excessive number of plasma cells produce abnormally high levels of these proteins, causing various symptoms and complications:
- Bone Pain and Fractures: The proliferation of myeloma cells damages bone tissue, leading to pain and an increased risk of fractures, particularly in the spine, ribs, and hips. This damage is often seen as osteolytic lesions.
- Anemia: Myeloma cells crowd out healthy blood cells in the bone marrow, resulting in anemia, which manifests as weakness, fatigue, and pallor.
- Kidney Issues: Elevated M-protein levels can damage the kidneys, leading to renal problems and symptoms like swelling in the legs due to fluid retention.
- Infections: A decrease in normal white blood cells increases the susceptibility to infections, such as pneumonia.
- Hypercalcemia: The destruction of bone releases calcium into the bloodstream, causing high calcium levels. Symptoms include confusion, excessive thirst, and changes in appetite.
Diagnosis and Treatment
Diagnosing multiple myeloma involves urine and blood tests to detect abnormal plasma cells and assess M-protein levels. The disease’s stage and subtype are crucial for determining treatment and prognosis. Prognostic factors include age, disease stage, and response to treatment. Advances in research and treatment have improved prognosis, though the disease remains complex and individualized. Multiple myeloma can lead to several complications affecting quality of life: Anemia, Leukopenia, Bone Erosion, High Blood Calcium Levels, Hyper viscosity.
While multiple myeloma currently has no cure, various treatment options are available to manage the disease effectively. Treatment goals include reducing M-protein levels, eliminating myeloma cells, improving quality of life with minimal side effects, and prolonging survival. Proteasome Inhibitors, Immunomodulatory Drugs, Monoclonal Antibodies against target Myeloma cells, Bispecific Antibodies which engage both engage both myeloma cells and immune cells, CAR T-Cell Therapy, Traditional Chemotherapy, Steroids are some of the primary treatment options. Supportive therapies address symptoms and treatment side effects, such as managing bone disease, kidney failure, and preventing blood clots. Radiation therapy can relieve pain and treat bone damage or solitary tumors. Complementary and adjunctive treatments may also be considered to improve patient well-being.
Understanding multiple myeloma requires a comprehensive approach to managing its impact on the body and exploring various treatment and supportive care options to enhance patient outcomes and quality of life. For more on therapeutics against this disease, stay tuned for M for Multiple Myeloma Part II. Meanwhile, click here for more available resources and support groups for multiple myeloma.
Dr. Malini Gupta, Ph.D.
Sources
- https://rarediseases.org/rare-diseases/multiple-myeloma/
- https://www.orpha.net/en/disease/detail/29073
- https://www.mdanderson.org/cancer-types/multiple-myeloma.html
- Figure inspiration : https://www.youtube.com/watch?app=desktop&v=ZFZptS3SlEw
- Graphic in the figure derived from: https://www.mskcc.org/cancer-care/types/multiple-myeloma
Disclaimer
The editors take care to share authentic information. In case of any discrepancies please write to newsletter@medness.org
The sponsors do not have any influence on the nature or kind of the news/analysis reported in MedNess. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of MedNess. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products as they are based only on very limited and dated open-source information. Assumptions made within the analysis are not reflective of the position of anyone volunteering or working for MedNess. This blog is strictly for news and information. It does not provide medical advice, diagnosis or treatment nor investment suggestions. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
MedNess is a part of STEMPeers® which is a 501(c)(3) organization registered in PA as PhD Career Support Group. The organization helps create a growing network of STEM scientists that is involved in peer-to-peer mentoring and support.



