Kennedy Disease, also known as Spinal Bulbar Muscular Atrophy (SBMA), is a rare X-linked recessive genetic progressive neuromuscular disease that causes muscle weakness and wasting (atrophy) throughout the body. Symptoms typically begin to appear between the ages of 30 and 50, with life expectancy being nearly normal. Males with the inherited gene usually develop symptoms, while females are generally carriers. A blood test can confirm if an individual has a SBMA CAG mutation, indicating a predisposition to developing the clinical symptoms associated with Kennedy’s Disease.
Kennedy Disease is caused by an unstable expansion of a CAG triplet repeat (40-62 repeats) in exon 1 of the androgen receptor (AR) gene on chromosome Xq11-12. This results in an expanded stretch of glutamines within the AR, leading to misfolding and proteolysis of the AR, making it insensitive to androgen hormones. In the nucleus, AR fragments aggregate, causing dysregulation of protein transcription and motor neuron degeneration. The loss of motor neurons impairs muscle contraction, resulting in progressive muscle wasting. A recently reported phenotype includes distal limb weakness and wasting due to mutations in the dynactin 1 (DCTN1) gene subunit.
Clinical Description and symptoms
| Classification Level | Disorder |
| Prevalence | 1/200, 000 |
| Age of Onset | Adult Onset |
| Inheritance | X-linked recessive |
Early symptoms include tremors, muscle cramps, muscle twitching, fatigue, and slurred speech. Symptoms can be categorized into neurological, muscular, thoracic, endocrine, geneto-urinary. Neurological symptoms include Issues with functions controlled by bulbar muscles (breathing, swallowing, talking), difficulty swallowing (a bulbar sign), hand tremors when performing tasks, abnormal response (toes bend up) indicates brain issues, muscle weakness and wasting due to loss of lower motor nerves, numbness and loss of sensation in certain areas. Muscular symptoms include muscle twitching without purposeful movement, large muscle spasms, muscle shakiness in certain positions, muscle wasting and shrinkage due to inadequate stimulation, thickened calf muscles due to cramps. Androgen Deficiency and estrogen excess. Increased apparent estrogen effects due to loss of masculinizing effects, erectile dysfunction, low sperm count, smaller, less functional testicles.
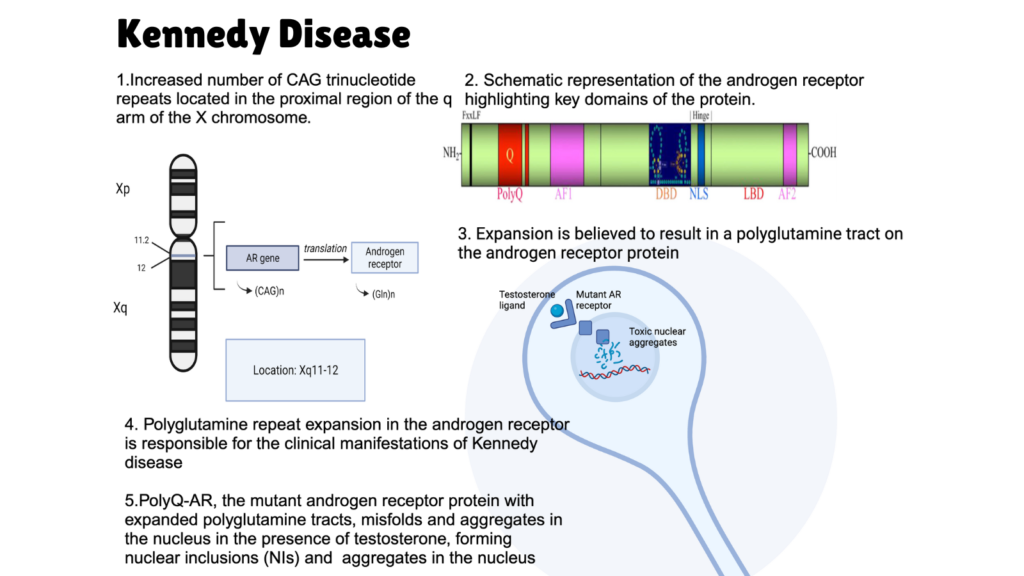
Image: Overview of Kennedy Disease; Image Source: Malini Gupta
Diagnosis and Current Treatment
Diagnosis of Kennedy Disease involves a detailed review of medical history, clinical examination, and specific tests such as elevated hormone levels and nerve conduction studies, along with genetic mutation confirmation, an example of such a service can be found here. Differential diagnoses include hereditary spastic paraplegia, spinocerebellar ataxia, other motor neuron diseases, myopathies, neuropathies, lead or aluminum poisoning, and cervical spondylosis. Antenatal diagnosis is possible for pregnant women who carry the mutation. Genetic counseling indicates that female carriers do not typically show symptoms but have a 50% chance of passing the mutation to their children, while affected men will ensure their daughters become carriers. Management includes symptomatic treatment with physiotherapy, medications, hormone therapy, and potentially surgery. Recent use of leuprorelin has shown benefits, and advanced cases may require tube feeding or respiratory support. The disease progresses slowly, with about one-third of patients needing a wheelchair 20 years after diagnosis. The overall prognosis is favorable, with only a slight decrease in life expectancy.
Currently, there is no known cure or treatment for KD, though research is ongoing. Some individuals manage symptoms with medications prescribed by their doctors, while others find relief through a light exercise and stretching program. For more on therapeutics against this disease, stay tuned for K for Kennedy Disease part II. Meanwhile, click here for more available resources and support groups for Kennedy’s Disease.
Dr. Malini Gupta, Ph.D.
Sources
- https://www.orpha.net/en/disease/detail/481
- https://kennedysdisease.org/
- https://rarediseases.info.nih.gov/diseases/6818/kennedy-disease
- https://rarediseases.org/rare-diseases/kennedy-disease/
- https://www.preventiongenetics.com/searchTests?val=SBMA
Disclaimer
The editors take care to share authentic information. In case of any discrepancies please write to newsletter@medness.org
The sponsors do not have any influence on the nature or kind of the news/analysis reported in MedNess. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of MedNess. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products as they are based only on very limited and dated open-source information. Assumptions made within the analysis are not reflective of the position of anyone volunteering or working for MedNess. This blog is strictly for news and information. It does not provide medical advice, diagnosis or treatment nor investment suggestions. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
MedNess is a part of STEMPeers® which is a 501(c)(3) organization registered in PA as PhD Career Support Group. The organization helps create a growing network of STEM scientists that is involved in peer-to-peer mentoring and support.



