Introduction
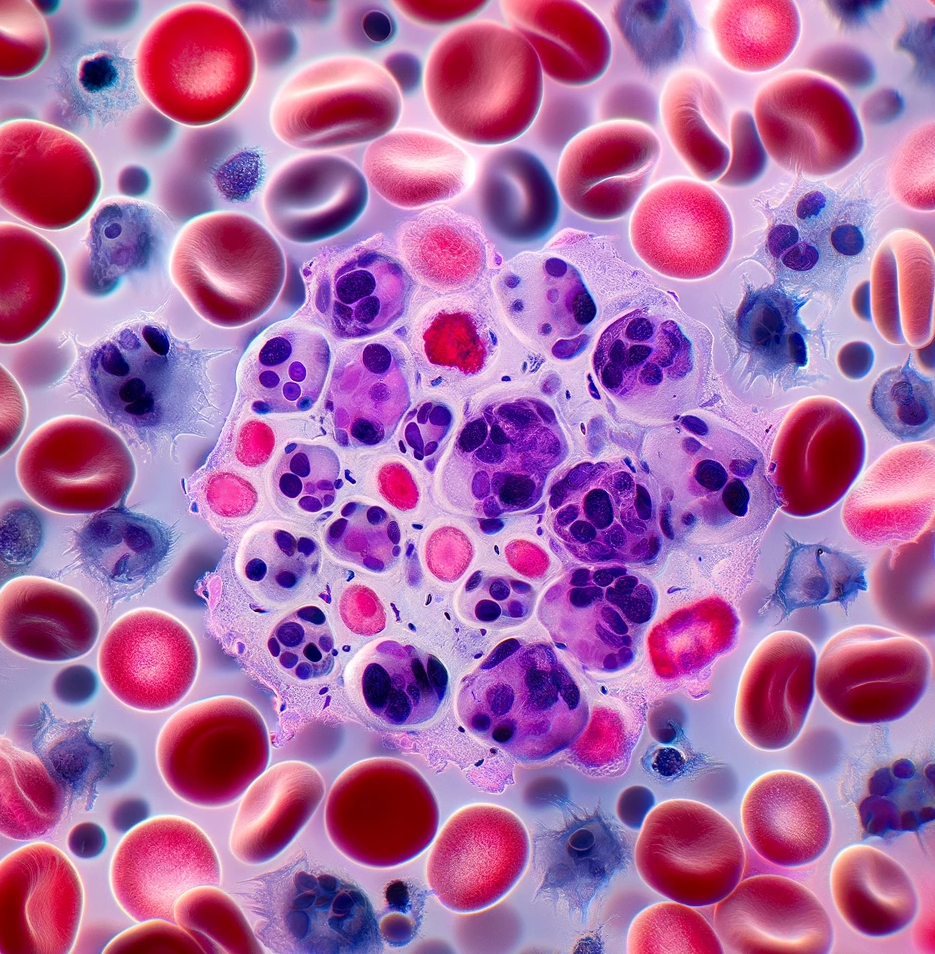
The FDA’s recent approval of obecabtagene autoleucel (Aucatzyl) marks a significant milestone in immunotherapy, offering hope for adults battling relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL). Developed by Autolus Inc., this CD19-directed, genetically modified autologous T-cell therapy targets a critical unmet need in hematologic oncology.
Current Regulatory Status
Obecabtagene autoleucel received FDA approval under expedited pathways, including regenerative medicine advanced therapy (RMAT) and orphan drug designations. These programs underscore its potential to address serious conditions with limited treatment options.
Drug and Technology Details
Aucatzyl employs chimeric antigen receptor (CAR)-T technology, where a patient’s T cells are harvested, genetically modified to express a CD19-specific receptor, and reinfused to target and destroy leukemia cells. The therapy is delivered in a split-dose regimen, tailored to the patient’s bone marrow blast levels and preceded by lymphodepleting chemotherapy with fludarabine and cyclophosphamide.
Trial Details
The approval was supported by data from the FELIX trial (NCT04404660), a single-arm, multicenter study evaluating 65 adults with relapsed or refractory CD19-positive B-cell ALL. Patients met stringent inclusion criteria, including disease relapse within 12 months or failure after multiple systemic therapies or stem cell transplantation.
Key efficacy outcomes included a complete remission (CR) rate of 42% within three months of infusion, with a median CR duration of 14.1 months. The overall response included complete remission and remission with incomplete hematologic recovery (CRi).
Safety Profile
While promising, the therapy comes with significant risks, as highlighted in its boxed warnings. Cytokine release syndrome (CRS) occurred in 75% of patients, with severe cases in 3%. Neurological toxicities, including immune effector cell-associated neurotoxicity syndrome (ICANS), were reported in 64%, with severe cases in 12%. Common adverse effects included infections, febrile neutropenia, fatigue, and gastrointestinal symptoms.
Conclusion
The approval of obecabtagene autoleucel represents a breakthrough in the treatment of relapsed or refractory B-cell precursor ALL, offering durable remission for patients with limited options. While its efficacy is remarkable, careful management of its risks will be essential for optimizing patient outcomes.
Dr. Vinoth Khandelwal, Ph.D.
Disclaimer
The editors take care to share authentic information. In case of any discrepancies please write to newsletter@medness.org
The sponsors do not have any influence on the nature or kind of the news/analysis reported in MedNess. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of MedNess. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products as they are based only on very limited and dated open-source information. Assumptions made within the analysis are not reflective of the position of anyone volunteering or working for MedNess. This blog is strictly for news and information. It does not provide medical advice, diagnosis or treatment nor investment suggestions. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
MedNess is a part of STEMPeers® which is a 501(c)(3) organization registered in PA as PhD Career Support Group. The organization helps create a growing network of STEM scientists that is involved in peer-to-peer mentoring and support.



