Progeria or Hutchinson-Gilford Progeria Syndrome (HGPS) is a rare and fatal genetic disorder characterized by premature aging that begins in childhood. The condition is typically not inherited but arises from a sporadic autosomal dominant mutation, with a low chance of occurrence (1 in 4 to 8 million), increasing to 2-3% if a family has already had one affected child due to mosaicism. Affected individuals experience growth delays, failure to thrive, and distinctive facial features, including a prominent forehead, protruding eyes, and a slender beaked nose. Skin issues such as hair loss, aged skin appearance, and loss of subcutaneous fat are also common. HGPS is caused by a mutation in the LMNA gene, which produces the Lamin A protein essential for maintaining nuclear integrity; this mutation leads to the production of an abnormal protein called Progerin. The exact cause of accelerated aging in HGPS is not fully understood but may be linked to cumulative cellular damage from metabolic processes and free radicals. Individuals with progeria often have reduced activity of antioxidant enzymes. Progerin accumulates in coronary arteries as people age, potentially contributing to atherosclerosis and serving as a marker for heart disease risk. Understanding and finding a cure for progeria could offer insights that benefit the wider population facing age-related health issues. HatsON for Progeria Day, is celebrated on April 7th every year.
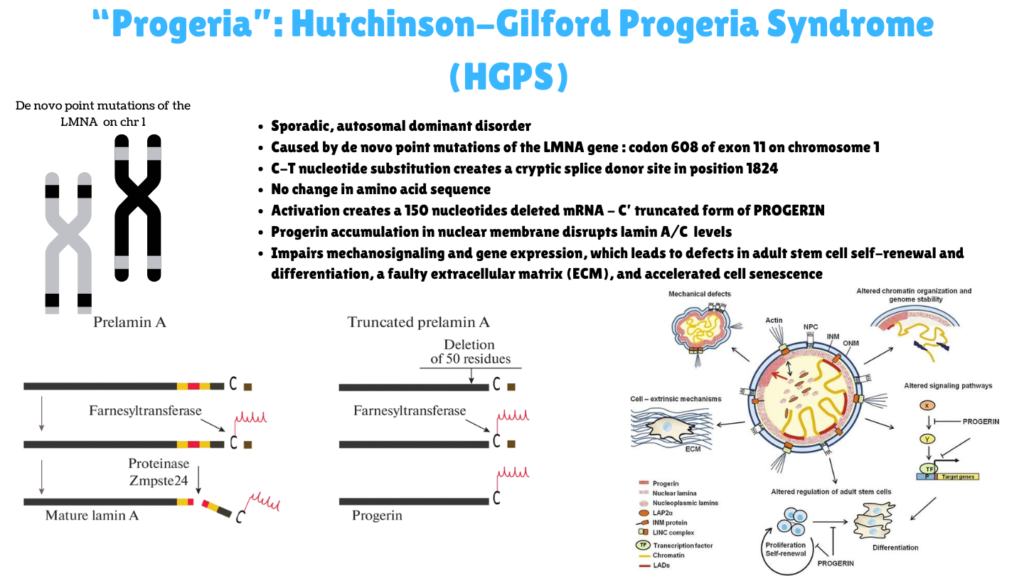
Image I: Causes and Effects of Hutchinson-Gilford Syndrome
Clinical Description, classification and symptoms
| Classification Level | Disorder |
| Prevalence | <1 / 1 000 000 |
| Age of Onset | Childhood, infacncy |
| Inheritance | Autosomal dominant, Autosomal recessive |
Children with Hutchinson-Gilford Progeria Syndrome (HGPS) may exhibit a range of symptoms, including a high-pitched voice, hearing loss, and early signs of arteriosclerosis, which can lead to serious cardiovascular issues like chest pain, heart failure, and heart attacks. Although they appear healthy at birth, signs of accelerated aging become evident within the first two years, including growth failure, loss of body fat and hair, aged-looking skin, joint stiffness, hip dislocations, widespread atherosclerosis, and strokes. Newborns may present with taut, shiny skin resembling scleroderma, midfacial cyanosis, and a sculpted nose. Skin abnormalities can involve a gradual reduction of subcutaneous fat, an aged appearance, and prominent veins, especially on the scalp and thighs. Nails may be thin, brittle, yellowish, or even absent. By age two, they typically show significant growth delays, often reaching a height like that of a three-year-old by age ten. As they grow, children with HGPS often develop underdeveloped facial bones, leading to a small face and prominent skull features, as well as dental issues like delayed tooth eruption and increased tooth decay.
Diagnosis and treatment
While there is no cure for Hutchinson-Gilford Progeria Syndrome (HGPS), regular monitoring and management can help address the condition. Medical visits typically include measuring weight and height, along with routine evaluations such as electrocardiograms, echocardiograms, imaging tests (X-rays and MRIs), and assessments of dental, vision, and hearing health.
Certain therapies may alleviate or slow the progression of symptoms. These include:
- Lonafarnib (Zokinvy): An oral medication that helps prevent progerin buildup, potentially extending lifespan.
- Low-dose aspirin: To reduce the risk of heart attacks and strokes.
- Other medications: Such as statins and blood thinners, depending on individual needs.
- Physical and occupational therapy to aid mobility and daily activities.
- Nutrition: A balanced, high-calorie diet, with supplements if needed.
- Assistive Devices: Hearing aids for those with hearing loss and eye care to manage dryness.
- Dental Care: Regular visits to a pediatric dentist to address common dental issues.
Understanding Progeria or HGPS requires a multidisciplinary approach tailored to the child’s specific symptoms can enhance quality of life and health outcome. For more on therapeutics against this disease, stay tuned for P for Progeria Part II. Meanwhile, click here for more available resources and support groups for Progeria. Read more on this rare disease here.
Dr. Malini Gupta, Ph.D.
Sources
- https://rarediseases.org/rare-diseases/hutchinson-gilford-progeria/
- https://www.progeriaresearch.org/
- https://www.orpha.net/en/disease/detail/740
- https://link.springer.com/article/10.1134/S0026893322020091#Fig3 – used in figure
- https://www.biospace.com/fda/us-fda-authorizes-launch-of-clinical-trial-to-support-new-treatment-development-for-progeria#
Disclaimer
The editors take care to share authentic information. In case of any discrepancies please write to newsletter@medness.org
The sponsors do not have any influence on the nature or kind of the news/analysis reported in MedNess. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of MedNess. Examples of analysis performed within this article are only examples. They should not be utilized in real-world analytic products as they are based only on very limited and dated open-source information. Assumptions made within the analysis are not reflective of the position of anyone volunteering or working for MedNess. This blog is strictly for news and information. It does not provide medical advice, diagnosis or treatment nor investment suggestions. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
MedNess is a part of STEMPeers® which is a 501(c)(3) organization registered in PA as PhD Career Support Group. The organization helps create a growing network of STEM scientists that is involved in peer-to-peer mentoring and support.



